
Social and behavioral determinants of perceived insufficient sleep. Grandner MA, Jackson NJ, Izci-Balserak B, et al. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Epidemiology of insomnia: what we know and what we still need to learn. Future multicenter clinical trials with large sample sizes are needed to validate its effectiveness in the Chinese population.Ĭ Identifier: NCT04779372. In this randomized clinical trial, the smartphone-based Chinese culture-adapted DCBT-I improved insomnia severity compared with sleep education. Some of the sleep diary measures and self-reported scales showed more improvements in the DCBT-I group than sleep education group, such as total sleep time (mean : 3 months, 403.9 minutes vs 363.2 minutes 6 months, 420.3 minutes vs 389.7 minutes) and sleep efficiency (mean : 3 months, 87.4% vs 76.7% 6 months, 87.5% vs 78.1% ). There were significant improvements from before to after the intervention for both the sleep education and DCBT-I groups, with large effect sizes(sleep education: d = 1.13 DCBT-I: d = 1.71). 048) and at the 3-month follow-up (12.1 points vs 14.8 points Cohen d = 0.489 P =. Mean (SD) ISI scores in the DCBT-I group were significantly lower than those in the sleep education group after the 6-week intervention (12.7 points vs 14.9 points Cohen d = 0.458 P =.

Cognitive behavioral therapy for insomnia full#
Of 82 participants (mean age, 49.67 years 61 females), with 41 randomized to sleep education and 41 randomized to DCBT-I 77 participants completed the 6-week intervention (39 participants in the sleep education group and 38 participants in the DCBT-I group full analysis data set) and 73 completed the 6-month follow-up (per protocol data set). Secondary and exploratory outcomes included sleep diary measures self-reported scales assessing dysfunctional beliefs about sleep, mental health, and quality of life and smart bracelet measures. The primary outcome was Insomnia Severity Index (ISI) scores with the intention-to-treat principle. Data were analyzed from January to February 2022.Ī Chinese smartphone-based app with the same interface was used in both DCBT-I and sleep education groups over 6 weeks, with 1-, 3-, and 6-month follow-ups. After assessing for eligibility, eligible participants were enrolled and allocated (1:1) to DCBT-I or sleep education groups. Follow-up visits were performed online or in the same hospital. Screening and randomization were conducted at Peking University First Hospital.
Cognitive behavioral therapy for insomnia trial#
This was a single-blinded, randomized clinical trial conducted from March 2021 to January 2022. To investigate the efficacy of a smartphone-based Chinese culture-adapted DCBT-I application (app) for insomnia compared with sleep education using the same app.
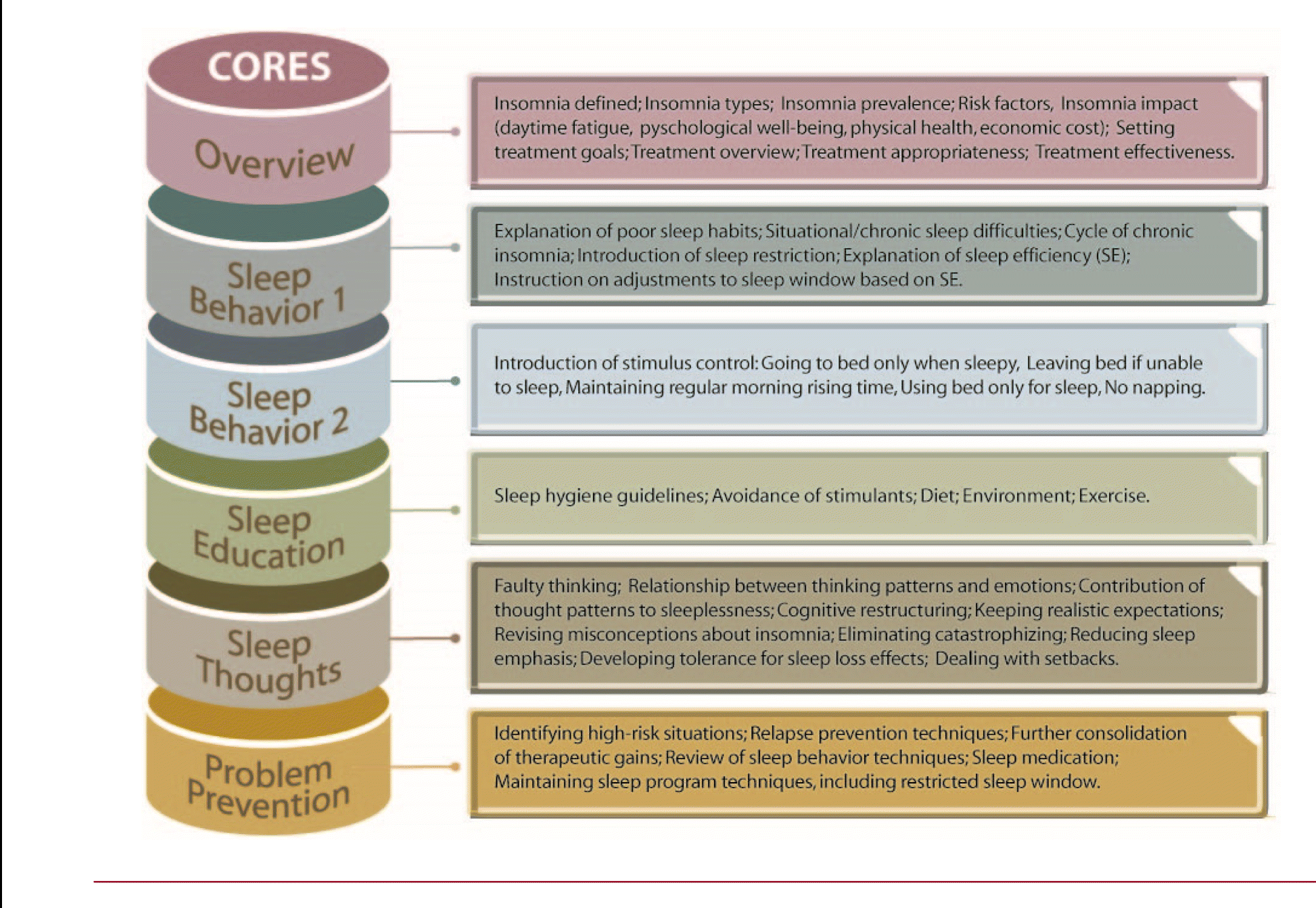
Moreover, studies comparing DCBT-I and sleep education in the same operating interface are lacking. Digital cognitive behavioral therapy for insomnia (DCBT-I) requires adaptation to different sociocultural contexts.


 0 kommentar(er)
0 kommentar(er)
